Atopic Dermatitis – Eczema in Adults
Introduction
What is Atopic Dermatitis (AD)/Eczema?
It is a long-term, itchy inflammatory skin disorder that typically affects the face (cheeks), neck, arms, and legs but usually spares the groin and axillary regions. It is commonly referred to as eczema.
Epidemiology
In the United States, the prevalence rate for atopic dermatitis (AD) is 10-12% in children and 0.9% in adults. Globally, it affects 15-30% of children and 2-10% of adults. It occurs in the first year of life in 85% of cases and occurs before age five in 95% of cases. The incidence is highest in early infancy and childhood. Furthermore, the disease may have periods of complete remission, particularly in adolescence, and may then recur in early adult life. In the adult population, the rate of AD frequency is 3% or higher, but onset may be delayed until adulthood.
What causes Atopic Dermatitis?
Atopic dermatitis usually occurs in people who have an ‘atopic tendency.’ Atopy refers to the tendency to asthma, eczema, and hay fever. Atopy is mostly inherited (genetic). It is characterized by an overactive immune response to environmental factors. This means that they react to particles (called allergens), which would be harmless to others. A bacterial infection or superimposed viral infection in a predisposed individual could trigger an inflammatory reaction. A typical agent is Staphylococcus aureus. Early exposure to allergens is said to help trigger the immune system to recognize allergens and produce corresponding antibodies. Extremes of climate can act as triggers. A dry atmosphere increases the tendency for dry skin. Also, sweating increases the tendency for itching. All of which can lead to AD. Also, Aeroallergens are various airborne substances or inhalants that can cause allergic disorders. Examples include pollens, spores, and other biological or non-biological airborne particles.
Signs and Symptoms
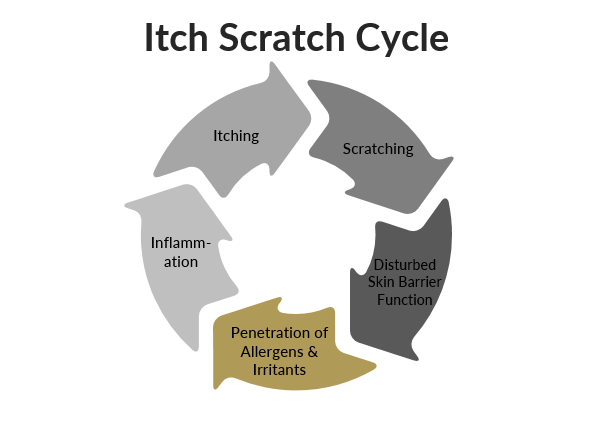
A common feature is itching. Some other factors can determine the clinical presentation, as well. These factors could be the presence of an additional skin condition or infection. Usually, itching starts even before the rash. The signs and symptoms vary according to age. In Infants, AD is usually noticed soon after birth. Dryness of skin occurs early and often involves the whole body. Although, in most cases, the diaper area and nose are usually spared. The most initial lesions affect the anterior aspect of the elbow and posterior aspect of the knee. Also, it may appear red and with discharge. Over the following few weeks, lesions usually localize to the cheeks, the forehead and scalp, and the lower legs. However, they may occur in any location on the body. The thickening of the skin is rarely seen in infancy.
Furthermore skin dryness is often generalized and is characteristic. It signifies repeated itching of the skin and is seen mostly over the elbow and knee regions, earlobes and eyelids, etc. The face appears pale; reddish and scaling occur around the eyes. Increased folds below the eye are often seen. Flexural creases are seen, particularly around the anterior aspect of the elbow and posterior aspect of the knee. Skin picking and hardening of the skin are frequent. They are likely to experience symptoms in their teens and beyond.
Also, In adults, lesions may present in various ways. The face is commonly involved and is dry and scaly. Skin dryness is prominent. Skin is often more thickened than in children. Usually, adults have persistent, localized eczema, possibly confined to the hands, eyelids, elbow and knee regions, nipples, or all of these areas.l
Atopic dermatitis usually occurs in people who have an 'atopic tendency.' Atopy refers to the tendency to asthma, eczema, and hay fever.
Treatment
Skin Care at Home
It is advisable to avoid scratching the skin and keep fingernails cut short. If nighttime scratching is a problem, consider using gloves. Take frequent lukewarm baths. Lubricate or moisturize the skin two to three times a day using ointments such as petroleum jelly. A humidifier in the home also can help. Also, avoid anything that worsens symptoms, including Irritants such as wool, strong soaps or detergents, and sudden changes in body temperature and stress, which may cause sweating. When washing or bathing: Keep water contact as brief as possible and use gentle body washes and cleansers instead of regular soaps.
Try to use mild cleansers such as Dove®, Cetaphil®, CeraVe®, Aveeno®, etc. which are less harsh on your skin.
Rarely do ‘moisturizing’ cleansers add moisture to your skin. Believing this leads people to overuse ‘moisturizing cleansers’ thinking that they are adding moisture when in fact they are only further stripping their skin of its own natural oils. Generally, a mild cleanser will simply be less harsh on the skin and strip less oil.
When a moisturizer is used, we recommend an unscented lotion or cream.
It’s best to apply within 3 minutes of getting out of the shower or bath.

Pharmacologic Therapy
Topical steroids like hydrocortisone are currently the mainstay of treatment. Ointment bases are preferred, particularly in dry environments. Second-line therapy includes immunomodulators such as Tacrolimus (Protopic®) and Pimecrolimus (Elidel ®). Topical phosphodiesterase-4 (PDE-4) such as Crisaborole (Eucrisa®) a topical ointment 2% is used for mild-to-moderate atopic dermatitis in adults and children aged two years or older).
Antihistamines like Diphenhydramine (Benadryl®) and Hydroxyzine (Atarax®) may help with sleep disturbance, but usually do not help much with the itching.
Also, targeted biologics like Dupilumab (Dupixent®) are both incredibly effective and have acceptable side effect profile. Oral Medications such Methotrexate, Cyclosporine, and JAK inhibitors have made eczema a manageable conditions for the most severely affected patients. Antibiotics are used for the treatment of clinical infection caused by S aureus or flares of disease. Pennsylvania Dermatology Specialists are your experts in diagnosis and management of atopic dermatitis, and can help come up with a plan that is safe, effective, and meets each individual patient’s needs.
Phototherapy
Phototherapy, as administed by Pennsylvania Dermatology Specialists (NBUVB) has been shown to be safe and effective for atopic dermatitis without any long term side effects or internal side effects. Please click here to learn more: Phototherapy

